Varicose veins are twisted and enlarged veins with a bluish appearance that often occur at the back of the knee, or on the lower leg and ankle. They can be one of the first visible signs of a chronic venous disease. This is defined as stage 2 according to an internationally accepted standard for describing patients with chronic venous disease (CEAP classification system).

What are varicose veins?
What causes varicose veins?
Varicose veins are usually caused by damaged vein walls and valves. The veins contain one-way valves that direct the blood flow to the heart and prevent it flowing backwards. If the vein valves are weakened or damaged, the blood can flow backwards and accumulate in the veins, causing them to stretch or twist. This leads to the typical appearance of varicose veins, which are visibly swollen and blue.
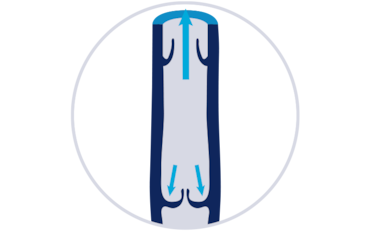
Valves working
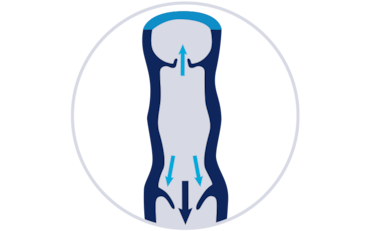
Valves nonworking
The following risk factors can impact the likelihood of developing varicose veins:
- Family history
- Personal medical history of blood clots
- Obesity
- Gender (women are more likely to develop the condition than men)
- Older age
- Long periods of standing or sitting
- Hormonal changes, e.g. pregnancy, birth control medication, or hormone replacement therapy
Many women notice varicose veins during pregnancy. Besides a pooling of blood in the legs and an increase of the blood volume in general, hormones can further weaken the vein walls during pregnancy.

Signs and symptoms of varicose veins
Varicose veins are often a cosmetic concern and don’t necessarily cause any other symptoms. However, in some cases when left untreated, they can develop in more severe stages of chronic venous disease. Varicose veins appear twisted and bulging, and are dark purple or blue in color, they can also lead to:
- Heavy and tired legs
- Achy feeling in the legs
- Muscle cramps in your legs at night, particularly in the calf muscles
- Dry and itchy skin in the affected area, which may sometimes be discolored
Varicose veins treatment options
Treatment options for varicose veins range from lifestyle changes to surgery. The treatment of varicose veins also depends on your general health, and on the size, location, and severity of the affected veins.
- Compression therapy:
Wearing compression stockings is an effective way to relieve symptoms. JOBST® has a range of medical compression stockings specially designed to counteract varicose veins and related symptoms. - Lifestyle changes:
Exercising regularly and elevating your legs when you sit or lie down is highly beneficial. Read more here. - Procedures:
Most procedures for varicose veins are done as outpatient procedures, which allow to leave the clinic or medical practice on the same day. - Endothermal ablation:
This procedure uses energy from high-frequency radio waves or laser to seal the affected veins. - Sclerotherapy:
A special foam is injected into the enlarged veins. This results in scarring and sealing of the affected veins. Ultrasound is usually used to visualize the location of the injection. - Ligation and stripping:
This procedure requires two small cuts– one near your groin at the top of the affected vein and another further down. The top of the vein is tied up and sealed. The affected vein is then removed via the second cut.
How to prevent varicose veins
Some risk factors that increase the likelihood of developing varicose veins can’t be controlled, such as age, gender, and family history. However, lifestyle changes can reduce the risk of varicose veins:
- Exercise regularly
- Maintain a healthy weight
- Wear flat shoes
- Avoid tight clothing around the waist, legs, and groin
- Avoid long periods of sitting or standing
- Take short breaks to raise the legs


